The New Yorker
On a recent Tuesday evening in London, the surgeon David Nott attended a dinner at Bluebird, an upscale Chelsea restaurant. The room was packed with doctors, renowned specialists who had come for the annual consultants’ dinner of the Chelsea and Westminster Hospital, one of Britain’s leading medical establishments. As waiters set down plates of lamb and risotto, Nott checked his phone and found a series of text messages. “Hi David,” it began. “This is an urgent consultation from inside Syria.” Attached was a photograph of a man who had been shot in the throat and the stomach.
The image had been sent by a young medical worker in Aleppo. He had removed several bullets from the patient’s small intestine, but he wasn’t sure what to do about the wound in the throat. For the past hour, the man had been slowly dying on the operating table while the medical worker awaited instructions.
“Sorry, didn’t see your message till now,” Nott typed under the table. “Is the neurology ok?” It was: a bullet had pierced the trachea and the esophagus, but it hadn’t damaged the spinal cord. Nott told the medical worker to insert a plastic tube into the bullet hole, to provide an even supply of air. Then, he instructed, sew up the digestive tract with a strong suture, and, “to buttress the repair,” partly detach one of the neck muscles and use it to cover the wound.
Nott returned to his lamb, which had gone cold. There were around fifty specialists in the room—many more than there are in the opposition-controlled half of Aleppo, where, in 2013 and 2014, Nott had trained medical students, residents, and general surgeons to carry out trauma surgeries far beyond their qualifications. Several had since been killed, and Nott often checked in with the others, especially when he saw reports that Syrian or Russian aircraft had attacked hospitals around the city.
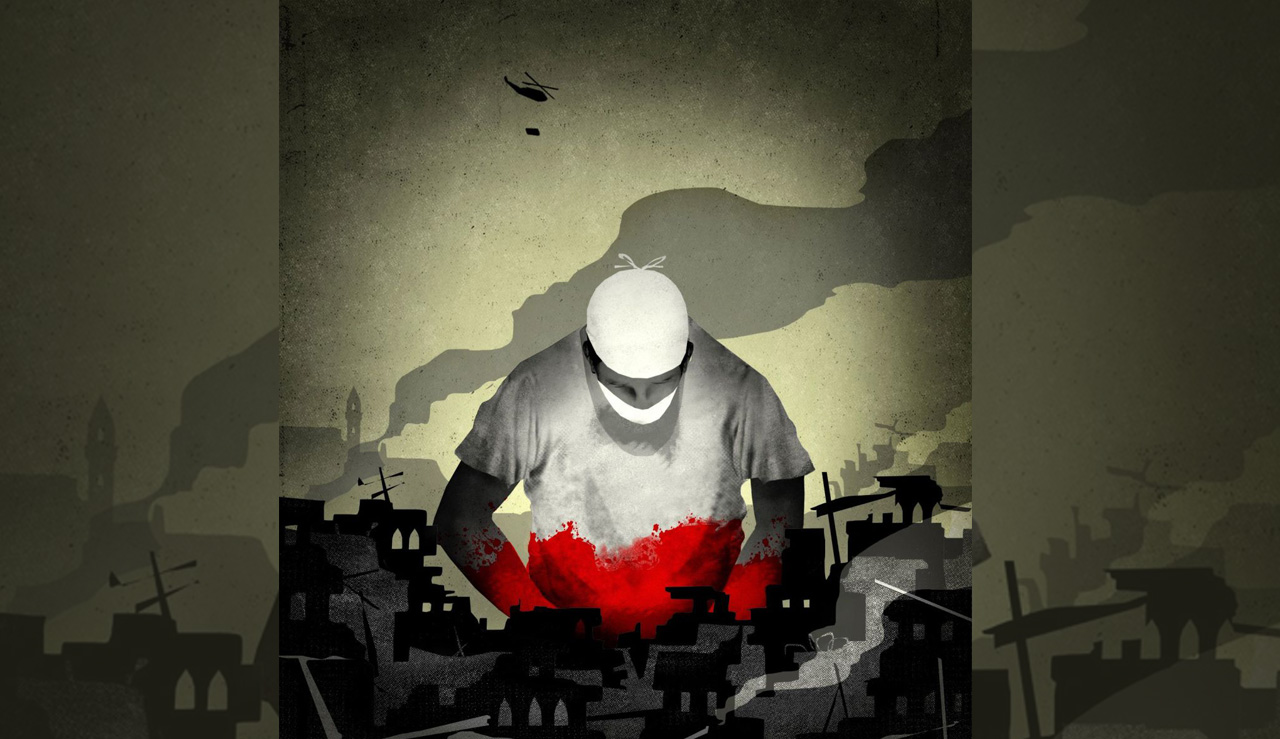
In the past five years, the Syrian government has assassinated, bombed, and tortured to death almost seven hundred medical personnel, according to Physicians for Human Rights, an organization that documents attacks on medical care in war zones. (Non-state actors, including isis, have killed twenty-seven.) Recent headlines announced the death of the last pediatrician in Aleppo, the last cardiologist in Hama. A United Nations commission concluded that “government forces deliberately target medical personnel to gain military advantage,” denying treatment to wounded fighters and civilians “as a matter of policy.”
Thousands of physicians once worked in Aleppo, formerly Syria’s most populous city, but the assault has resulted in an exodus of ninety-five per cent of them to neighboring countries and to Europe. Across Syria, millions of civilians have no access to care for chronic illnesses, and the health ministry routinely prevents U.N. convoys from delivering medicines and surgical supplies to besieged areas. In meetings, the U.N. Security Council “strongly condemns” such violations of international humanitarian law. In practice, however, four of its five permanent members support coalitions that attack hospitals in Syria, Yemen, and Sudan. The conditions in Syria have led to a growing sense among medical workers in other conflict zones that they, too, may be targeted.
Despite the onslaught, doctors and international N.G.O.s have forged an elaborate network of underground hospitals throughout Syria. They have installed cameras in intensive-care units, so that doctors abroad can monitor patients by Skype and direct technicians to administer proper treatment. In besieged areas, they have adapted hospitals to run on fuel from animal waste. Nott, for his part, trained almost every trauma surgeon on the opposition side of Aleppo, as part of a daring effort to spread medical knowledge as the government strives to eradicate it.
As a child, Nott constructed hundreds of model airplanes from kits and from scratch, and hung them from the ceiling of his bedroom, in Worcester. His dream was to fly commercial jets, and in secondary school he earned his pilot’s license. But his father, an Indo-Burmese surgeon who had married a British nurse, wanted him to become a doctor. “He used to sit there in my room, forcing me to learn,” Nott told me when I visited him at his private clinic in London, last month. Nott, who is fifty-nine, speaks softly, and has a calm, professorial demeanor. In 1978, he enrolled in the medical program at Manchester University, where he marvelled at human anatomy. “The most exciting machine is a human being,” he said. “It’s actually the same as an airplane or a helicopter. They both have an engine. They both require fuel.”
Shortly before Christmas in 1993, Nott was working as a general surgeon at Charing Cross Hospital, in London, when he saw a television report from Sarajevo. For twenty months, the city had been under siege by the Bosnian Serb Army, and the program showed a field hospital in need of staff. The next day, Nott volunteered with Médecins Sans Frontières, and on Christmas Eve he left for a three-month stay in Sarajevo, where he worked at a facility that had been so severely damaged by shelling and sniper fire that people called it Swiss Cheese Hospital.
After that trip, Nott took long periods of unpaid leave from his jobs at various London hospitals to volunteer for humanitarian-aid agencies in other areas afflicted by war and natural disaster. He operated on thousands of patients in more than twenty countries—including Afghanistan, Sierra Leone, Haiti, and Nepal—often with rudimentary equipment and insufficient supplies of medication and donor blood. The conditions forced him to learn an array of surgical techniques that in London would all have been carried out by different specialists.
In 2008, on the day that Nott arrived at an M.S.F. hospital in Rutshuru, in the Democratic Republic of the Congo, he found a sixteen-year-old orphan whose arm had been improperly amputated. The stump was infected, and the muscles were gangrenous. Without a forequarter amputation—a complicated procedure in which the entire shoulder is removed, usually as a last resort to halt the spread of cancer—the boy would die. Nott had never done the operation, so he sent a text message to Meirion Thomas, who was Lead Surgeon at the Royal Marsden Hospital, in London. Minutes later, Thomas replied, “Start on clavicle. Remove middle third.” He sent nine more steps, and signed off, “Easy!” The boy recovered.
At the time, military doctors in Iraq and Afghanistan were adopting a transformative approach to the worst battlefield-trauma cases. Typically, surgeons treated life-threatening abdominal bleeds from gunshots and bomb blasts by cutting open the abdomen, searching for the damaged organs and arteries, repairing them, and stitching up the incisions. The fixes could take hours, and patients often died on the operating table after their body temperature plummeted.
American and British military surgeons started practicing “damage-control surgery,” an established concept that hadn’t been applied in combat zones. Practitioners do the absolute minimum to stop the bleeding and prevent sepsis before sending patients to the intensive-care unit for warming, fluids, and resuscitation. The patient returns to the operating theatre only when his body is stable enough to handle hours under the knife.
“I wanted to be a part of this surgical revolution,” Nott told me. “And the only way to do that is actually to be there, to get the case in front of you. You can’t read it in a book.” He volunteered as a surgeon with the Royal Air Force and was quickly deployed to Basra, in Iraq, and later to Camp Bastion, in Afghanistan. At Camp Bastion, in 2010, “we had a thousand and seventeen major trauma cases in six weeks,” he recalled. “It was people with their arms and legs blown off. It was people shot in the head, people shot in the chest, people with fragmentation injuries everywhere.” Two years later, Queen Elizabeth II awarded Nott the title of Officer of the Order of the British Empire for his medical work in war zones.
In the first weeks of March, 2011, the start of the insurrection in Syria, the security forces of President Bashar al-Assad detained and tortured children who had drawn anti-regime slogans on a wall in the southern city of Dara’a. Tens of thousands of protesters took to the streets, and on March 22nd Assad’s forces stormed into the city hospital, kicked out the nonessential medical staff, and positioned snipers on the roof. Early the next morning, the snipers fired at protesters. A cardiologist named Ali al-Mahameed was shot in the head and the chest as he tried to reach the wounded. Thousands of people attended his funeral, later that day, and they, too, were attacked with live ammunition. For the next two years, the snipers remained stationed on the roof, “firing on sick and wounded persons attempting to approach the hospital entrance,” according to the U.N. commission.
As protests erupted all over the country, government-run hospitals basically functioned as an extension of the security apparatus, targeting demonstrators who dared to seek treatment. “Some doctors manage to treat simple cases and manage to let them flee without being seen or registered,” one doctor said, in testimony collected by Médecins Sans Frontières. “But if an admission is required for the patient, then the administration of the hospital is notified, and therefore it reaches security.” Pro-regime medical staff routinely performed amputations for minor injuries, as a form of punishment. Many wounded protesters were taken from the wards by security and intelligence agents, sometimes while under anesthesia. Others didn’t make it as far as the hospital; security agents commandeered ambulances and took the patients straight to intelligence branches, where they were interrogated and often tortured and killed. M.S.F. concluded that, for Syrians who opposed the President, the health-care system was “a weapon of persecution.”
In response, some doctors established secret medical units to treat people injured in the crackdown. One surgeon at Aleppo University Hospital adopted the code name Dr. White. Along with three colleagues, he identified and stocked safe houses where emergency operations could be performed. Dr. White also lectured at the university’s faculty of medicine; he suspected that seven of his most promising students shared his sympathies toward the nascent uprising. Another doctor, named Noor, recruited them to join the mission. In Arabic, noor means “light,” so the group called itself Light of Life.
At night, Noor and Dr. White gave the medical students lessons via Skype, concealing their faces and voices. The goal was to teach them the principles of emergency first aid, with an emphasis on halting the bleeding from gunshot wounds. During demonstrations, the students waited in cars and vans to shuttle injured protesters to the safe houses, then disappeared. “They had to leave the house before my arrival,” Dr. White told me during a recent Skype call from Aleppo. “They could not know who this man is.”
Similar covert medical networks sprouted up all over Syria. But the safe houses were equipped with little more than gauze, cotton, and serum. One doctor told M.S.F., “When we receive serious casualties—a patient who needs to be hospitalized—we have two options: either we let him die or we send him to hospital not knowing what will become of him.”
In the first year of the uprising, Physicians for Human Rights documented fifty-six cases of medical workers being targeted by government snipers; tortured to death in detention facilities; shot and set on fire while driving ambulances; and murdered by security agents at checkpoints, in their clinics, or at home. Several were killed while treating patients. In July, 2012, the regime enacted a new terrorism law, making it an offense to fail to report anti-government activity; according to the U.N. commission, this “effectively criminalized medical aid to the opposition.”
That summer, Noor, the founder of Light of Life, was kidnapped at his clinic by security agents and later killed. Three of Dr. White’s students were also abducted; their charred corpses were found the following week. “From that day, I changed my name another time,” he told me. “I became Abdul Aziz”—the name he uses today.
“Your room is exactly how you left it before you went to college, except, of course, for our boarder, Mr. Grunze.”
In June, 2012, M.S.F. surreptitiously opened its first Syrian field hospital, in Atmeh, a rebel-held village near the Turkish border. For a year, the organization had been asking the Assad regime for permission to operate in the country, to no avail. The hospital, code-named Alpha, was set up in six days, in a walled villa that had been donated by a local doctor. In September, 2012, David Nott travelled to Alpha with other M.S.F. staff from around the world. To make space for patients, the doctors slept on the roof, where they often heard explosions and watched jets streaking through the sky. After each attack, taxis and pickup trucks collected casualties and sped toward the villa.
Natalie Roberts, an M.S.F. doctor from Wales, directed the emergency room. “Often, a lot of patients would arrive at once,” she told me. She stood at the gate, directing the less urgent cases toward beds on the shaded patio and the worst cases inside. As she began emergency treatment, Syrian staff members managed the crowd forming at the gate, turning away friends and family members who wanted to enter. The scene was always tense and emotional, Roberts said. “Sometimes they’d arrive with dead bodies, and we’d just have to say that there’s nothing we can do.”
The dining room served as a holding area for the most serious cases, which Roberts rated Red or Yellow on triage forms. Red patients needed to go into the operating theatre—at Alpha, this was the kitchen—within the hour; Yellow patients could survive for as long as four hours without surgery; the walking wounded were marked Green. Compared with other facilities in Syria, the M.S.F. hospital was well stocked, with surgical supplies filling the kitchen cabinets. Even so, Nott told me, “when someone comes in Red, the surgeon must ask, ‘Do I have enough resources to operate on him?’ If I don’t, the patient is going to go into the Black Zone,” which means he’s going to die, and there’s no point wasting supplies to try to save him.
Every trauma center requires a large supply of fresh blood. A person has about eleven pints, and, “if you’ve lost six pints, then your heart doesn’t get enough oxygen, and your brain doesn’t get enough oxygen,” Nott explained. “That’s why you collapse and go into a coma.” In Atmeh, when the facility ran out of blood, a nearby mosque broadcast a call for donors, and locals lined up outside. Elsewhere in Syria, doctors donated their own blood, while the recipient lay on the operating table.
One day, a half-dozen people were delivered to Alpha hospital in a truck, some dead, some badly wounded. Roberts was perplexed; usually, large groups arrived only after jets had bombed houses, and she hadn’t heard any planes that day. According to Nott, one of the wounded men was a rebel who, while fashioning makeshift grenades at home, had accidentally blown up his wife and child. In the operating room, the doctors cut away his pants, and Nott took a photograph of the scene, which he showed me last month, in London. “If you look here,” he said, pointing to the man’s sagging pants pocket, “there’s the other bomb.” The doctors found it when it dropped to the floor with a terrifying clink.
Inside the operating theatre, Nott often wore a GoPro camera, which he used to make surgical-training videos; for the past decade, he had been training doctors who work in conflict zones, and after six weeks in Syria he returned to London with thousands of images of grisly wounds from Alpha. Many of the victims were old men, women, and children, including a young boy who had picked up a cluster bomb that blew off his hands, and a nine-year-old girl hit by shell fragments, whose intestines dangled from her body.
As rebels captured territory, Roberts followed the front line deeper into Syria, visiting secret medical facilities and assessing their needs. Opposition fighters controlled significant portions of northern Syria, including the eastern half of Aleppo and several villages connecting it to the Turkish border. Roberts helped set up hospitals inside a cave in Idlib and a basement in Al Bab, as well as a blood bank and a vaccination program in Aleppo. However, she told me, “we couldn’t find qualified doctors,” especially in rural areas.
By late 2012, a number of Syrian expatriates had established medical charities. Although they sent aid and ambulances from Turkey into Syria, they rarely coördinated their efforts. “It was really chaotic,” Roberts said. “You would turn up at a pharmacy with a kit of antibiotics to donate and find that they already had massive quantities of the same drug. And then you would go to another hospital and realize that they had practically no help at all, because the hospital manager didn’t have experience working with international organizations.” At that point, she said, the facilities that received support were “the ones that were shouting the loudest.”
To handle the logistics, Aziz, of Light of Life, formed a group called the Aleppo City Medical Council. There were eight main medical facilities, and, with only twenty physicians and a handful of surgical specialists in the opposition-held half of the city, the staff used walkie-talkies to coördinate the distribution of patients. To evade detection, the doctors established sequential code names for each hospital, M1 through M8. Most of the staff had little, if any, formal training.
Eventually, the doctors built other medical centers and gave them random names, like M20 and M30, to obscure the actual number of targets. According to Aziz, the best location for a medical facility is on a narrow street, flanked by tall buildings, so that, after an air strike, helicopters and jets have difficulty tracking the movement of wounded civilians. Ambulance workers were routinely targeted by snipers and helicopters, so many of them removed sirens and medical logos, and coated their vans with mud. At night, they drove with the headlights off.
By the end of 2012, Syrian government forces had attacked medical outposts at least eighty-nine times, in eight provinces. Near Damascus, they raided and burned to the ground a clinic and three hospitals, killing all the patients and staff in one of them. In Homs, they shelled a field hospital twenty times in two days. In Aleppo, military aircraft fired rockets at a children’s hospital, causing it to shut down. Ground forces spent four days shelling a mental hospital. M1 was bombed twice, M2 once, and M4, which was attacked at least four times, finally collapsed in a pile of concrete and twisted metal, crushing to death several patients and staff.
In early 2013, Nott gave a presentation at the Royal Society of Medicine about M.S.F.’s work in Syria. After the lecture, he sat with Mounir Hakimi, a doctor who is the vice-chairman of a charity called Syria Relief, based in Manchester. Nott and Hakimi had met once before, at Alpha hospital, in Atmeh: when the Syrian doctor who had donated the villa was wounded by shrapnel, Nott treated him in his own former kitchen, and Hakimi came to pick him up. But, because Hakimi wasn’t a patient, Nott wouldn’t let him inside the operating theatre, and they got into a shouting match. Now, at the lecture, Nott said, “I realized he was quite a nice chap.” Hakimi, who had befriended Aziz, suggested that Nott travel to Aleppo with Syria Relief.
That August, in London, Nott led a five-day surgical-training course for around thirty-five doctors who work in “austere environments” all over the world. Hakimi attended, along with Ammar Darwish, another Syrian doctor living in the U.K. The next month, Nott, Hakimi, and Darwish set off for Aleppo.
Outside the entrance to M1, there was a large decontamination tent fitted with showers to rinse off victims of chemical attacks. A few weeks earlier, Syrian government forces had fired sarin-gas rockets into densely populated neighborhoods of Damascus, killing some fourteen hundred people; Western governments spoke of retaliation, but they quickly retreated, and since then the regime has habitually used chlorine as a weapon. On roads leading to the hospital, signs on lampposts listed chemical-attack survival tips. Aziz drove Nott to Aleppo, and introduced him to the medical staff at M1, where he lived for the next five weeks.
The emergency department at M1 was run by medical students. “Before David arrived, no one knew how to cut open a chest,” Abu Waseem, a young medical worker specializing in plastic and reconstructive surgery, told me. On Nott’s second day in Aleppo, a sixteen-year-old boy was carried into the operating room without a heartbeat. While one Syrian physician conducted chest compressions, another sliced open the abdomen, to check for internal bleeding. The guts were intact. Nott checked on the operation and realized that the boy’s heart had been pierced by shrapnel. Abu Waseem and the others crowded around the operating table to watch Nott work.
Nott grabbed a scalpel and cut between two ribs. Then he inserted a Finochietto retractor—a stainless-steel crank that, in the age of laparoscopic surgery, looks practically medieval—and spread apart the ribs to gain access to the heart, which had a hole in the right ventricle. He told one of the Syrians to reach into the cavity and pump it with his hands. Soon, the heart started functioning, spurting blood into the air with each contraction. Nott stitched up the heart as it was beating, and the boy survived.
“There were a lot of things that we didn’t know how to deal with,” Aziz told me. “If I had a patient with thoracic trauma, I didn’t know how to fix him, because I wasn’t a thoracic surgeon. If I had a patient with vascular injuries, I used to send him to another hospital, where there was a vascular surgeon.” He added, “Most of the cardiac injuries died.”
In the evenings, as the sun set and the shooting let up, Nott taught his course on surgery in austere environments. (Darwish translated the lectures into Arabic.) He showed hundreds of surgical photographs and videos that he had taken in distant war and disaster zones, including examples of his own deadly mistakes. He also distributed digital copies of several hundred medical textbooks. In London, he had chopped off the bindings with an industrial paper cutter and run each page through a scanner.
Nott taught the physicians to move flaps of muscle and skin to cover exposed bone and open wounds. One day, he saw a man whose hand had been completely flayed. In lieu of amputation, he sewed the hand to a flap in the man’s groin, which slowly sealed itself around the bones of the hand. After three weeks, Abu Waseem cut away the connective tissue, donating a large chunk of flesh to a hand that would otherwise have rotted. In vascular surgery, the circulatory system can be treated as a series of interchangeable tubes; when vital blood vessels were irreparably damaged, Nott sliced superficial veins out of healthy limbs and swapped them in for arteries. He did the same with injured nerves.
Nott also taught the physicians the principles of damage-control surgery, which he had learned at the bases in Iraq and Afghanistan. Because damage-control surgery calls for only minimal surgical fixes on the first pass, the practice allowed the Syrian doctors to tend to more patients after large-scale attacks. “It made a revolution in our work,” Aziz told me. “Real changes. So many patients survived because of these techniques.”
Some surgeons at M2 and M10 travelled to M1 for Nott’s evening lectures. At the end of each class, the Syrians discussed the cases that had come in that day—“who lived, who died, and why they lived, and why they died,” Nott said. “And then, because we’d get air-to-ground missiles after dark, we’d still have patients coming in. I’d carry on operating until midnight. And it would go on like that every single day.”
M1 is in the neighborhood of Bustan al-Qasr, a few hundred yards from the only crossing point between the rebel and the regime sides of the city. (The route has since been closed.) Each day, thousands of locals crossed from one side to the other to buy food, visit relatives, and take school exams. Corrupt fighters on the rebel side extorted those desperate to cross; snipers on the regime side used the alley for target practice. Bystanders who dared to retrieve the victims were often shot, too.
“Every day, we’d receive about twelve to fifteen sniper wounds,” Nott told me. Many of the victims were children, and the patients coming in from the crossing point arrived with eerily consistent injuries. “It was very strange,” Nott said. “You’d know that, at the start of the day, if you got a patient shot in the right arm, you’d have six or seven more shot in the right arm. And if somebody got shot in the abdomen you’d have six or seven shot in the abdomen.” Nott suspected that snipers were targeting specific areas of the body, as part of a sadistic game. He consulted with Aziz, who claimed that the gunmen were making bets over whom they could hit, and where. Aziz told me, “We used to sometimes listen to the walkie-talkies of the regime. And they used to listen to us.” One day, he said, “we heard a man say, ‘I bet for a box of cigarettes . . .’ ”
Even pregnant women were targeted, the doctors suspected. “This is a pregnant lady who’s just about to deliver,” Nott explained, in London, as he clicked through a series of ghastly photographs on his laptop. “She was forty weeks pregnant and was about to have a breech delivery, and was shot in the uterus.” A Syrian physician filmed Nott performing an emergency Cesarean section. Only the mother lived; an X-ray of the fetus showed a bullet lodged in its skull.
Nott was under constant threat of abduction. isis had already kidnapped sixteen foreign journalists and aid workers, and the Syrian government had captured another British doctor in Aleppo, an orthopedic surgeon named Abbas Khan, who later died in a prison cell in Damascus. Humanitarian doctors treat patients regardless of their loyalties, and, one day, as Nott was sewing up the artery that connected a man’s heart and lungs, “the doors of the operating theatre just flew open, and we had about seven isis fighters come in,” he said. They stood at the door, Kalashnikovs drawn. The leader, a Chechen, approached the table. The patient was one of his troops. Abu Abdullah, a young Syrian surgeon, stepped forward and told the man, in English, that if he disturbed the senior surgeon “your friend will die.” Nott shook with fear. “I was trying to concentrate on my hands so much that I could hardly stand,” he said. A commotion outside drew the guards away, but the leader stayed until the operation was complete. A month after Nott left M1, the same group of fighters returned and kidnapped a patient who had been wounded in both legs. They dragged him down the stairs, deposited him in the middle of the street, and executed him.
In January, 2014, isis kidnapped thirteen doctors from an M.S.F. field hospital in northern Syria. Eight were Syrian, and they were soon released, but the five foreigners remained hostages until the end of May. M.S.F. shut down its operations in isis-held areas and withdrew its foreign staff from the country.
Nott returned to M1 in September, 2014. Every hospital in the opposition-held eastern half of the city had been attacked. At M10, pieces of ceiling, glass, and concrete covered broken beds in a former ward, while a leftover bag of serum dangled near an electrical outlet. Medical staff at both facilities crammed equipment and patients into the basements and stacked sandbags around the entrances. The upper floors were deserted, serving only as shields against bombardment.
For almost a year, Syrian government helicopters had been lobbing barrels filled with shrapnel and TNT onto markets, apartment blocks, schools, and hospitals. Welded tail fins guide the barrels to land on top of an impact fuse. The methods of targeting are so rudimentary and indiscriminate that, in Aleppo, many residents have moved closer to the front lines, risking sniper fire and shelling, because the helicopters don’t drop barrels near government troops.
When a large bomb explodes, it destroys bodies in consecutive waves. The first is the blast wave, which spreads air particles at supersonic speeds. This can inflict internal damage on the organs, because, Nott said, “the air-tissue interface will bleed. So your lungs start to bleed inside. You can’t breathe. You can’t hear anything, because your eardrums are all blown out.” A fraction of a second later comes the blast wind, a negative pressure that catapults people into the air and slams them into whatever walls or objects are around. “The blast wind is so strong that in the wrong place it will actually blow off your leg,” Nott said. He showed me a photograph of a man on the operating table, whose left leg was charred mush and mostly missing below the knee. “It’ll strip everything off your leg. And that’s why people have such terrible injuries. It’s the blast wind that does that, followed by fragmentation injuries,” from bits of metal shrapnel that rip through flesh and bone, and the flame front, which burns people to death.
In the aftermath of a barrel-bomb attack, Nott said, “as you walked down the stairs to the emergency department, you just heard screams.” Barrel bombs blow up entire buildings, filling the air with concrete dust; many people who survive the initial explosion die of suffocation minutes later. Every day, patients arrived at the hospital so mangled and coated in debris that “you wouldn’t know whether you were looking at the front or the back, whether they were alive or dead,” he said. “Every time you touched somebody, the dust would go into your face and down into your lungs, and you’d be coughing and spluttering away as you were trying to assess whether this patient was alive.”
The tiled floor of the underground emergency department at M1 was slick with blood and other fluids. Screaming men carried in headless children, as if they could somehow be saved. Hospital staffers wrapped corpses in white shrouds and stacked detached legs that still wore socks and shoes.
When barrel bombs fall on homes, they often send entire families to the ward. One day, five siblings arrived. Unable to treat any of them, Nott started filming the scene, so that he would have proof, he said, of “how terrible it was.” A baby with no feet let out a stifled cry, then died. An older brother lay silently nearby, his guts coming out. In the next room, a toddler with blood on his face shouted the name of his dying brother. Two medical workers carried in the fourth brother, who was about three years old. His pelvis was missing, and his face and chest were gray with concrete dust. He opened his eyes and looked around the room, blinking, without making a noise. There were wet, white blobs on his face, and Nott gently wiped them away. When the sister was brought into the room, he learned that a concrete block had fallen on her head, and the blobs were pieces of her brain.
The boy was dying. There was no treatment; he had lost too much blood, and his lungs had filled with concrete particles. Nott held his hand for four agonizing minutes. “All you can do is just comfort them,” he told me. I asked him what that entailed, since M1 had exhausted its supply of morphine. He began to cry, and said, “All you can hope is that they die quickly.”
A few weeks after Nott left Aleppo, he was invited to lunch at Buckingham Palace. Wild duck and vintage port were served. Janet Oldroyd Hulme, one of Britain’s most prolific growers of rhubarb, sat on his left, and the Queen sat on his right. When the Queen turned to him, he explained that he had just returned from Syria. “How was it?” she asked. “I tried to play it light, and I said it was absolutely dreadful,” he told me. The Queen pressed for details, but he couldn’t bring himself to tell her, and his bottom lip began quivering. At that point, “she summoned the corgis,” he said. For the next twenty minutes, Nott and the Queen petted the dogs and fed them biscuits under the table. As the lunch came to a close, he says, she remarked, “That’s much better than talking, isn’t it" ?
Since Nott’s last trip to Aleppo, Syrian government forces have dropped barrel bombs on all three trauma hospitals in the city. In separate missile strikes, they killed several of Nott’s friends, including an anesthetic technician and a paramedic. Physicians for Human Rights has catalogued and corroborated three hundred and sixty-five attacks against Syrian medical facilities, more than ninety per cent of which were perpetrated by Syrian and Russian government forces. Many of them are “double-tap” strikes: around twenty minutes after the first bomb falls, a helicopter or a jet returns to the scene and blows up the rescuers.
In the first week of June, Syrian and Russian aircraft carried out more than six hundred air strikes on the opposition side of Aleppo, and Assad vowed to take back “every inch” of Syria. The next day, pro-Assad warplanes bombed three medical facilities, including a health center for newborn babies, in the span of three hours. M2, M3, M4, M6, M7, and M9 have been destroyed.
Aziz told me that, in the opposition-held half of Aleppo, there are now five general surgeons, two or three orthopedic surgeons, one obstetrician, and one anesthesiologist. “I’m a general surgeon working as a thoracic surgeon, working as a cardiac surgeon, working as a vascular surgeon, sometimes doing ultrasounds, sometimes doing X-rays,” he said. “And it’s the same for the rest of the guys. He is a nurse? He became an intensive-care technician. He is a worker in the hospital? He became an operating-room technician, because he learned how to deal with sterilization, how to deal with surgical equipment.”
“If you go to Aleppo and ask the doctors in any hospital, they will tell you that since David Nott came to Aleppo, there was a huge leap forward in the performance of medical practice,” Ammar Darwish told me. “He’s still saving lives down there, because he taught these doctors how to do a good job.”
Nott continues to advise the medical staff at M1 from afar. Earlier this year, he and his wife, Elly, a former Middle East researcher at the International Institute for Strategic Studies, started a foundation to run surgical-training courses for doctors who live in war zones. In April, he and Darwish travelled to southern Turkey for the first session, held at a university in Gaziantep. Thirty-two Syrians attended, coming from Aleppo, Idlib, Homs, and Latakia provinces.
One of Nott’s best students is Abu Waseem. When the war began, he was a fourth-year plastic- and reconstructive-surgery resident at a government hospital. “He sacrificed his future” to continue treating patients in Syria, Aziz told me. “He has no way to graduate, no way to do his fifth or sixth year and become a specialist.” While other physicians in Aleppo take frequent breaks and visit family members who have escaped to Turkey, Abu Waseem remains at M1, because he doesn’t have a passport.
Nott often asks Abu Waseem how he’s coping. Not long ago, he replied, “Thank you, my friend, I am fine. But I am so sad.” He sent two photographs of a young child with horrific injuries. “Look at this girl. This is one of the victims of a Russian bombing today. She lost her whole arm and her face.”
“Terrible,” Nott wrote back. “Is she going to survive?”